A couple of years ago, the UCSF Fresno Department of Psychiatry began using webcams for outpatient care and training purposes. The early implementation of such equipment has been a godsend in the pandemic, allowing outpatient training to continue with residents seeing patients in video sessions rather than in their offices to prevent potential exposure risks to COVID-19.
A 30-45-minute session with a patient in a small office is a high-risk interaction and UCSF Fresno halted outpatient training for residents last March when the COVID-19 pandemic started. Luckily, outpatient resident training was not disrupted for long because computer video equipment was available at University Psychiatry Associates (UPA), the faculty practice and residency training clinic. The pandemic had forced physician practices across the country to pivot to telemedicine and seemingly overnight, webcams became a scarce commodity. “You couldn’t buy them,” said Craig C. Campbell, MD, program director, UCSF Fresno Psychiatry Residency. “But we already had the equipment that we needed so we didn’t really skip a beat.”
Within two weeks of stopping in-person sessions, UCSF Fresno had converted 100% to telehealth psychiatry with help from Central California Faculty Medical Group (CCFMG) in securing a telehealth platform for the video sessions, Dr. Campbell said. “We had a lot of luck and tremendous support from CCFMG and their leadership and their IT (Information Technology). They made us look good, they made us look nimble,” he said.
It was important that training and care not be interrupted. The San Joaquin Valley has among the lowest per capita ratios of behavioral health professionals to the population, according to the UCSF Healthforce Center. UCSF Fresno residents provide much needed mental health care while in training and about 60% of the UCSF Fresno residents remain in the region at completion of residency, Dr. Campbell said.
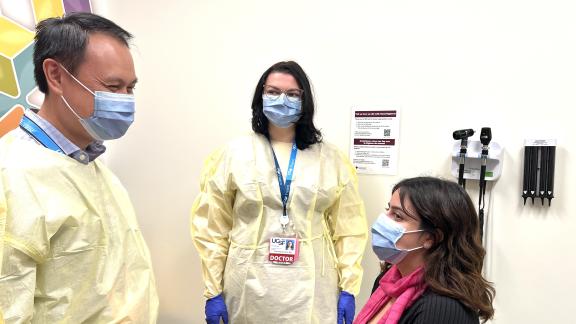
The challenge has been adapting faculty supervision protocols to an outpatient training model. Residents now connect with patients by logging into the telehealth system, and faculty can join sessions virtually for purposes of clinical oversight. During the early months of the pandemic, residents worked out of the UPA offices, but in the late fall, as COVID-19 cases surged, all residents began working from their homes.
“All of sudden, you’re working with patients and residents over a Zoom link, Dr. Campbell said. “Most of it has been a very steep, hands on learning curve; and I was learning right along with residents and with my patients, along with supervising residents’ work.”
This year, the UCSF Fresno Department of Psychiatry has a complement of 24 residents (six residents across four years, which completes a four-year expansion to increase class size in the department from four residents to six per class. Residents have adjusted to telemedicine but some have embraced it more than others, Dr. Campbell said.
Fourth-year resident who grew up in Fresno, Lisa Wise, MD, found it difficult to find suitable space to hold telemedicine sessions at home. Her 7-year-old son is online-learning at home so she opted to come into her office at UPA for telemedicine sessions. For some patients, finding a confidential space in which to have a session also has been a challenge, Dr. Wise said. “We (residents) had to catch on pretty quickly to ask ‘are you in a place where you can talk now? Is anyone else in the home with you?’”
Patients overall have been accepting of telemedicine, she said. For some, telehealth is more convenient, especially for those with transportation issues or who live far from the clinic. For others, however, an unfamiliarity with the technology has been an obstacle and some patients, especially among the elderly population have no internet connection, requiring telephone sessions. Surprisingly, these have gone well, Dr. Wise said. “Patients can feel self-conscious on video but talking on the telephone can help for some patients”, she said. “There’s a sense of anonymity and some open up about things they might not on video or even in person.” For others, particularly very paranoid patients, they might imagine others are in the room with you listening to the conversation and feel more guarded.
Before the pandemic, the UCSF Fresno Department of Psychiatry offered telemedicine as an elective for residents in their fourth year. Given an option, Dr. Wise said she would not have chosen telemedicine, but under the circumstances, she said, “I see it as a necessary part of training. We all need to understand how to do this now.”
Telemedicine was a big change, said Nicholas Betchel, DO, a third-year resident who grew up in the Central Valley and who plans to remain after residency. “We really relied on Dr. Campbell to navigate us through this,” he said. “And as a resident, I felt very cared for throughout all of this. They (UCSF Fresno) found the resources needed and provided them to us. Dr. Betchel has become comfortable using telemedicine and is open-minded about incorporating it into a practice in the future. “Patient outcomes haven’t worsened,” he said. “I’ve had some really good outcomes with video therapy and medication management.”
Residents who began their second year at UCSF Fresno in January were doing inpatient rotations when the pandemic started and have experienced only telemedicine in their outpatient training. Andrew Shiovitz, MD, a second-year resident, is thankful he does not have to worry about exposure to COVID-19 and of bringing the virus home to his pregnant wife and toddler son. Telemedicine is not without flaws. “But as long as COVID-19 is going to be a concern, I think this is the best thing to make sure we’re adept at doing this,” he said. As for whether he will prefer outpatient telemedicine over in-person sessions, it is too soon to tell, Dr. Shiovitz said. “This to me is outpatient work. I have nothing else to compare it to.”
As COVID-19 cases decrease and more people are vaccinated for the coronavirus, the need for training residents in telemedicine loses some urgency, but “very few people expect things to return to 100% pre-pandemic status,” Dr. Campbell said. People who have difficulty traveling to a clinic are very appreciative of telemedicine and are hoping it remains an option, even when the pandemic is over, he said. UCSF Fresno’s Department of Psychiatry is well-prepared for training physicians to provide excellent patient care by telemedicine to serve patients through this pandemic and beyond.